Improving Prescriber Practices
One of the most productive places to reduce the risk of harm through opioid use and misuse is through improved prescribing of these beneficial but potentially harmful medications. A nuanced approach to examining prescribing data is needed. Depicting overall opiate prescription rates is not sufficient for improving prescriber practices; as we demonstrate, drilling down further into the data is essential. Beyond examining data, collaborative decision-making with patients is needed – where providers communicate with patients about their pain control needs.
Providers should avoid prescribing narcotic pain relievers whenever possible – and even then, the lowest dosage for the shortest duration possible is prudent[16]. Furthermore, there are patients for whom opiates should not be dispensed as the first choice for managing pain; this includes patients who are at high risk for addiction. There are many different types of pain control options, including multidisciplinary and multimodal efforts that include rehabilitation therapy, and non-opioid analgesics. A broad perspective on approaches to pain control should be adopted[17].
Another subgroup of patients in need of careful monitoring for appropriateness of ongoing medication use are those who are already receiving opiates and are requesting a refill. For patients requesting refills of opiate prescriptions, this may be an opportune time to cease or taper the dosage. A stated treatment goal should be to avoid dependence on opiates[18] and avoid switching to other habit-forming drugs.Yet another subgroup of patients includes those who have chronic pain, for whom other therapies have failed. Carefully tailored treatment plans are in order to address patient needs for chronic pain relief. There are clinical practice guidelines for pain control in chronic pain non-cancer patients [19]. Although some chronic pain patients may already be managed using long-term opioid therapy (LTOT), it is important for providers to work with patients so that there is not an expectation that they will be pain-free; staying within a tolerable threshold of pain should be the therapeutic goal. For LTOT patients, it’s particularly important to take an interdisciplinary approach – with careful monitoring to be sure clinical guidelines are being followed.
Patient Engagement around the issue of pain management and opiate avoidance can be challenging, particularly if patients have experienced benefits from the medication. A primary goal of improving provider practices should be to avoid having appropriate pain management develop into drug dependence. Providers must engage in conversations with their patients about what non-narcotic solutions will be acceptable to manage pain[20]. Ideally, prescribers should work with pharmacists on the care team to carefully monitor opiate prescriptions. Pharmacists contribute much expertise which can help in forming an acceptable pharmacologic solution; this may be an iterative process of adjusting dosages and formulations until an appropriate pain control solution is reached.
In addition to using your in-house EHR data, some states have established prescription drug monitoring programs (PDMPs)[21], and have databases that could be used to examine prescriber opioid practices. This is an improvement on traditional utilization management approaches. Accessing information from a clearinghouse (other examples may include health information exchanges [HIEs], pharmacy insurance claims, etc.) will allow a broader view of prescriber and patient activity and can be useful to help providers make the most informed choice for what is best for the patient.
Conclusions
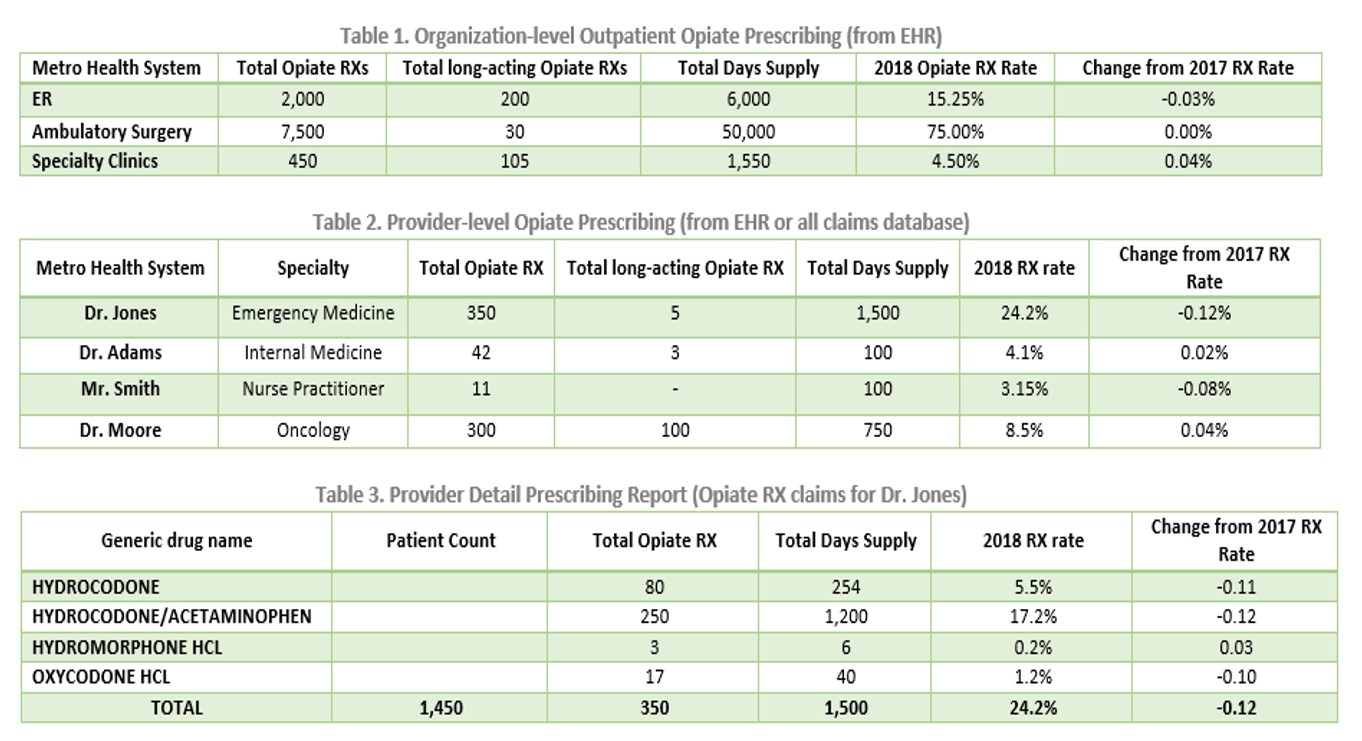
Sum-IT Health Analytics provides custom analytic solutions to align with your patient care methodologies and clinical workflows. These solutions leverage your prescribing data and turn it into actionable information that can be used to improve prescriber practices. We compare observed prescribing to the relevant clinical practice guidelines to identify areas for intervention. Some prescribers may have high proportions of patients for whom they prescribe opiates; furthermore, some providers may prescribe long duration or high dosages of MME for their patients (e.g., fentanyl). All of these prescribing practices should be examined to reduce the risk of harm to patients.
Health organizations need actionable data: which providers, which patients, which medications may require modification? Making this information available to providers is an effective tool for improving prescriber practices[22]. We need to assist providers to employ alternative (non-narcotic) pain management strategies ensure that patients are using addictive drugs for only very short time frames. There is an inherent need for providers to work with patients to achieve pain control, however we must work toward non-narcotic options.
Contact us to learn more about how we can collaborate with your organization to improve prescribing practices.
Contact Sum-IT or the authors at:
Miriam Isola, DrPH, CPHIMS Kathy Schneider, PhD
847-975-2141 515-771-3981
Co-Founder and Chief Strategy Officer Co-Founder and Epidemiologist
Miriam.Isola@sumithealthanalytics.com Kathy.Schneider@sumithealthanalytics.com
http://www.sumithealthanalytics.com/
[1] Dahlhamer J, Lucas J, Zelaya, C, et al. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults — United States, 2016. MMWR Morb Mortal Wkly Rep 2018;67:1001–1006. DOI: http://dx.doi.org/10.15585/mmwr.mm6736a2external icon.
[2] Institute of Medicine. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press; 2011. https://www.nap.edu/read/13172/chapter/1
[3] U.S. Drug Enforcement Administration, Office of Diversion Control. (2015). National Forensic Laboratory Information System Special Report: Opiates and Related Drugs Reported in NFLIS, 2009–2014. Springfield, VA: U.S. Drug Enforcement Administration. https://www.deadiversion.usdoj.gov/nflis/spec_rpt_opioids_2014.pdf
[4] Guy GP Jr., Zhang K, Bohm MK, et al. Vital Signs: Changes in Opioid Prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017;66:697–704. DOI: http://dx.doi.org/10.15585/mmwr.mm6626a4
[5] Increases in Drug and Opioid Overdose Deaths — United States, 2000–2014. January 1, 2016 / 64(50);1378-82. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm
[6] Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and Opioid-Involved Overdose Deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Rep 2019;67:1419–1427. DOI: http://dx.doi.org/10.15585/mmwr.mm675152e1
[7] Owens PL, Barrett ML, Weiss AJ, Washington RE, Kronick R. Hospital Inpatient Utilization Related to Opioid Overuse Among Adults, 1993-2012. HCUP Statistical Brief #177. August 2014. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb177-Hospitalizations-for-Opioid-Overuse.pdf.
[8] Weiss AJ, Bailey MK, O’Malley L, Barrett ML, Elixhauser A, Steiner CA. Patient Characteristics of Opioid-Related Inpatient Stays and Emergency Department Visits Nationally and by State, 2014. HCUP Statistical Brief #224. June 2017. Agency for Healthcare Research and Quality, Rockville, MD. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb224-Patient-Characteristics-Opioid-Hospital-Stays-ED-Visits-by-State.pdf
[9] HCUP Fast Stats. Healthcare Cost and Utilization Project (HCUP). April 2019. Agency for Healthcare Research and Quality, Rockville, MDhttps://www.hcup-us.ahrq.gov/faststats/OpioidUseServlet?radio-3=on&location1=US&characteristic1=01&setting1=ED&location2=&characteristic2=01&setting2=IP&expansionInfoState=hide&dataTablesState=hide&definitionsState=hide&exportState=hide Accessed 7/27/2019.
[10] Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The DAWN Report: Highlights of the 2011 Drug Abuse Warning Network (DAWN) Findings on Drug-Related Emergency Department Visits. Rockville, MD. https://www.samhsa.gov/data/sites/default/files/DAWN127/DAWN127/sr127-DAWN-highlights.htm
[11] Food and Drug Administration. “Timeline of Selected FDA Activities and Significant Events Addressing Opioid Misuse and Abuse.” https://www.fda.gov/drugs/information-drug-class/timeline-selected-fda-activities-and-significant-events-addressing-opioid-misuse-and-abuse . Downloaded 7/4/2019.
[12] US HHC “Opioids: The Prescription Drug & Heroin Overdose Epidemic.” Webpage. https://www.hhs.gov/opioids/
[13] Bree Collaborative. “Prescribing Opioids for Postoperative Pain – Supplemental Guide.” July 2018. http://www.agencymeddirectors.wa.gov/Files/FinalSupBreeAMDGPostopPain091318wcover.pdf
[14] Qaseem A, Wilt TJ, McLean RM and Forciea MA. “Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians.” Ann Int Med. 2017;166(7):514-530. DOI: 10.7326/M16-2367
[15] Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR Recomm Rep 2016;65(No. RR-1):1–49. DOI: http://dx.doi.org/10.15585/mmwr.rr6501e1external icon.
[16] Pino CA and Covington M. “Prescription of opioids for acute pain in opiate naïve patients.” UpToDate. May 14, 2019. https://www.uptodate.com/contents/prescription-of-opioids-for-acute-pain-in-opioid-naive-patients. Accessed 7/18/2019.
[17] Kroenke K, Alford DP, Argoff C, Canlas B, Covington E et al. “Challenges with Implementing the Centers for Disease Control and Prevention Opioid Guideline: A Consensus Panel Report.” Pain Medicine 2019; 20(4): 724-735. doi: 10.1093/pm/pny307
[18] American Psychiatric Association. Opioid Use Disorder. https://www.psychiatry.org/patients-families/addiction/opioid-use-disorder/opioid-use-disorder. Accessed 7/19/2019.
[19] Califf RM, Woodcock J and Ostroff S. “Special Report: A Proactive Response to Prescription Opioid Abuse.” NEJM, April 14, 2016; 374(15): 1480- 1485.
[20] Kroenke K, et al. op. cit.
[21] Centers for Disease Control and Prevention. What States Need to Know about PDMPs. https://www.cdc.gov/drugoverdose/pdmp/states.html . Accessed 7/27/2019.
[22] Partnership for Health IT Patient Safety. Safe Practice Recommendations for Safer Opioid Prescribing: Measures and Clinical Decision Support. White paper. ECRI Institute& HIMSS, 2019. https://assets.ecri.org/PDF/HIT-Partnership/EHRA-ECRI-Safe-Opioid-White-Paper-Final.pdf